“The only man who behaves sensibly is my tailor; he takes my measurements anew, every time he sees me, while all the rest go on with their old measurements and expect me to fit them”. -George Bernard Shaw
Cranium is a fixed space, containing brain tissue, CSF, and blood. In an adult, total inracranial volume is 1475 ml. This consists of 1300 ml brain parenchyma, 65 ml if CSF and 110 ml of blood.
Intracranial pressure (ICP) is, pressure exerted by the cranial content, on dura mater. Pressure is built by, arterial flux and depends on the volume, and therefore partial pressure, of each component of skull's content.
ICP = P brain + P blood + P csf
If one component pressure of ICP increases (for example, if brain oedema develops and 'P brain' increases), other component pressures should decrease, to keep ICP constant, as per Monro Kellie doctrine.
Compensatory mechanism to keep ICP constant, are:
▪ Shift of CSF from ventricular/ subarachnoid space into spinal compartment,
▪ Removal of blood from cerebral venous sinuses,
▪ Increased CSF absorption.
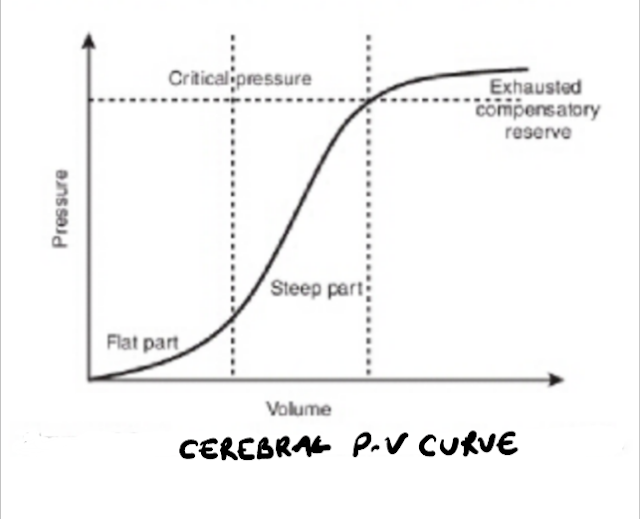
Intracranial space has limited capacitance, that is, only a small increase in volume of any compartment, may increase ICP. This relation is reflected in cerebral pressure volume curve also.
ICP monitoring consists of ICP pulse waveform, Cerebral PV curve and derived indices, Cerebral perfusion pressure, RAP and PRx.
●ICP PULSE WAVEFORM:
It is a modified arterial pressure waveform. ICP waveform has three distinct components.
▪The first peak (P1) is 'percussive' wave, and is due to arterial pressure being transmitted, from choroid plexus to the ventricle. It is sharply peaked and fairly consistent in amplitude.
▪The second wave (P2), called 'tidal' wave, is due to brain tissue compliance. It is variable, indicating changing cerebral tissue compliance. It increases in amplitude as compliance decreases. If it's amplitudes exceeds that of P1 waveform, cerebral compliance is markedly reduced.
▪Third waveform (P3) is due to closure of aortic valve, representing dicrotic notch in arterial pressure waveform.
Normally amplitude of P1>P2> P3.
Both amplitude and shape of ICP pulse waveform changes, if compliance decreases. As compliance reduces, P2 amplitude becomes larger than P1. A gentle pressure on abdomen, if causes increase in P2 amplitude or mean ICP, reflects reduced intracranial compliance.
●CEREBRAL PRESSURE VOLUME CURVE (PV CURVE):
Relationships between ICP and intracranial volume is non linear. Compliance decreases as intracranial volume increases. Three zones can be identified on PV curve-
1. Good compensatory reserve- it is the initial flat part of PV curve. It reflects good compliance, where a change in volume brings about no or minimal change in pressure. This happens as CSF is displaced into spinal compartment and blood is displaced from cerebral venous sinuses.
2. Poor compensatory reserve- this is the middle steep part of PV curve. A further increase in volume, may produce rapid and marked increase in pressure. This occurs as compensatory mechanism are depleted.
3. Exhausted compensatory reserve- this is the last flat part of PV curve. It reflects a high ICP, where it equals MAP.
● CEREBRAL PERFUSION PRESSURE (CPP):
CPP = MAP - ICP
●RAP (CORRELATION COEFFICIENT BETWEEN AMPLITUDE AND PRESSURE):
RAP reflects the compensatory reserve of intracranial compartment.
It is derived by calculating linear correlation between consecutive, time avaraged (6-10 seconds) data points of the amplitude of fundamental components and ICP (about 40 samples). RAP indicates where on the PV curve, the system is working.
RAP is measured from -1 to +1. If it is near 0, there is good PV compensatory reserve, and a volume change produces no or minimal change in ICP.
When RAP increases to +1, compensatory reserve is low, meaning any further increase in volume may cause a rapid increase in ICP.
IF RAP decreases to less than 0, it indicates compromised cerebrovascular autoregulation. High ICP prevents transmission of arterial pulse pressure to intracranial compartment, thus felling RAP to below 0.
During ICP monitoring, a change of RAP from +1 to 0 or negative indicates rise in ICP above critical level and irreversible brain injury may occur. However, fall in RAP from +1 to 0, after decompressive craniotomy reflects recovery of good compensatory reserve. A low averaged RAP is associated with worsened outcome, independent of ICP.
●PRx ( PRESSURE REACTIVITY INDEX ):
PRx measures relationship between ICP and MAP and reflects cerebrovascular autoregulatory reserve. It is calculated by correlation coefficient between 30-40 consequative time avaraged ICP and MAP data points obtained at 10 second interval.
PRx ranges between +1 to -1. A negative (-1 to 0) value indicates no correlation between ICP and MAP, translating into preserved cerebrovascular autoregulation.
Whereas a Positive PRx (0 to +1) indicates a positive correlation between ICP and MAP, reflecting impaired autoregulation.
Abnormal PRx values are associated with poor outcome after TBI.
Return of PRx to negative value after decompressive craniotomy reflects return of cerebrovascular autoregulation.
●Rule to remenber:
One of the rule in critical care is, shape is more important than number in every monitoring system. ICP waveform shape/ configuration give more information than the number.
ICP pulse waveform amplitude, index of comebsatory reserve (RAP), pressure reactivity index (PRx) can be used to guide therapy, even if number is normal.
●INDICATION OF ICP MONITORING:
•Moderate to severe TBI, who cannot be serially assessed,
•Severe TBI and abnormal CT brain,
•Severe TBI and normal CT brain but any two of folliwing- age >40, SBP <90, abnormal motor posturing.
●ICP MONITORING DEVICES:
it can be divided by site of placement and type of catheter.
•Site of placement- Intraventricular, Intraparenchymal and Subdural.
•Type of Catheter- Hollow fibre and Fibre optic.
Hollow fibre catheter has advantage of draining csf and reducing ICP as well as transducer can be zeroed after insertion. But it is associated with increased chances of infection. It can be placed only intraventricular space. It is preference where external ventricular drainage is needed.
Fibre optic catheter has built in microprocessor and can be placed in all three places. It has less infectious complication compared to hollow fibre catheter. But once inserted it can not be zeroed (zero drift phenomenon).
ICP monitoring therefore has, not only, diagnostic and therapeutic implications, it is of great helps in prognostication also.

Comments
Post a Comment